Millions of individuals worldwide suffer from the painful and incapacitating medical ailment known as pancreatitis. We will examine the definition, pathophysiology, kinds, stages, causes, risk factors, signs and symptoms, investigations, general therapy, prevention, and dietary recommendations associated to pancreatitis in this extensive beginner’s guide. We will also discuss the possible advantages of homeopathy as a different approach to treating pancreatitis.
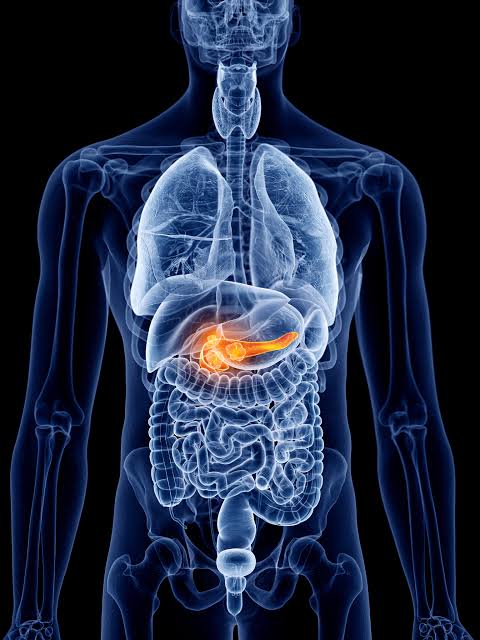
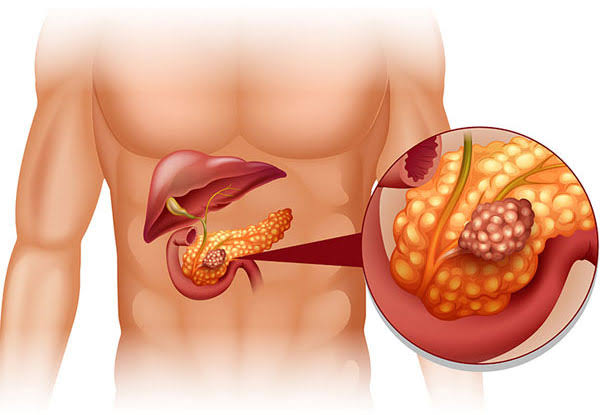
Understanding Pancreatitis
The ailment known as pancreatitis is typified by pancreatic inflammation. As the primary producer of hormones and digestive enzymes, including insulin, the pancreas is a vital organ in the digestive system. An inflammation of the pancreas can result in several health problems.
Tracing the Pathology of Pancreatitis
The pancreas’ own self-digestion due to the activation of its digestive enzymes frequently results in pancreatitis, an inflammatory condition. This can be an unpleasant and harmful procedure that impairs the pancreas’ ability to function normally.
The Various Types of Pancreatitis
There are two primary types of Pancreatitis:
1. Acute pancreatitis: This type of pancreatitis usually manifests quickly and lasts only a short while. It can be mild, moderate, severe, or even potentially fatal in extreme circumstances.
2. Chronic pancreatitis: In contrast to acute pancreatitis, this kind of pancreatitis is a chronic illness marked by a slow and ongoing inflammation of the organ. It may result in irreversible harm to the organ and its capabilities.
The Stages of Pancreatitis
Depending on how severe it is, pancreatitis can be divided into several stages:
1. Mild: With the right medical attention, most individuals recover from this stage, but there may be some localized inflammation.
2. Moderate: Pseudocysts and infections are among the more serious complications of moderate pancreatitis. Intensive care and hospitalization are frequently needed.
3. Severe: This is a dangerous stage of pancreatitis that can result in organ failure and potentially fatal consequences.
How Does Pancreatitis Happen?
The most common causes of pancreatitis include:
1. Gallstones: An inflammation-causing blockage of the pancreatic duct can result from gallstones.
2. Alcohol Consumption: The pancreas can get irritated and damaged by excessive alcohol consumption.
3. Trauma: An abdominal injury may be the cause of pancreatitis.
4. Infections: Both bacterial and viral infections may be a factor in the illness.
What Puts the Pancreas at Risk?
Several risk factors increase the likelihood of developing pancreatitis, including:
1. Excessive Alcohol Use: Drinking alcohol continuously poses a serious risk.
2. Obesity: A higher incidence of pancreatitis is associated with being overweight or obese.
3. Smoking: There is a link between smoking and a higher risk of pancreatitis.
4. Family History: An increased risk may be associated with a family history of pancreatitis or related disorders.
5. Specific Drugs: Certain drugs have the potential to make people more susceptible to pancreatitis.
Signs and Symptoms of Pancreatitis
Pancreatitis can manifest various signs and symptoms, including:
1. Abdominal Discomfort: One of the main signs of pancreatitis is severe, discomfort in the upper abdomen.
2. Nausea and Vomiting: These symptoms are frequently brought on by the inflammation of the pancreas, which disrupts digestion.
3. Fever: A high body temperature could be a sign of a pancreatitis-related infection.
4. Jaundice: When the bile duct is impacted by inflammation, yellowing of the skin and eyes may result.
5. Digestive Problems: Pancreatitis might result in nutritional malabsorption and diarrhea.
Investigations for Pancreatitis
Diagnosing pancreatitis involves various tests, including:
1. Blood Tests: Pancreatitis may be indicated by elevated pancreatic enzyme levels.
2. Imaging: The pancreas and surrounding structures can be seen through CT and MRI studies.
3. Endoscopic Ultrasound: This makes it possible to examine the pancreas and its ducts up close.
General Management of Pancreatitis
The treatment approach for pancreatitis often includes:
1. Hospitalization: In order to monitor and treat severe instances, hospitalization is necessary.
2. Pain Management: The purpose of medications is to reduce discomfort and pain.
3. Replacement of Fluids and Nutrients: Patients may need nutritional assistance and IV fluids.
4. Treatment of Underlying Causes: Dealing with the underlying issue, such as getting rid of gallstones or giving up alcohol.
General Prevention of Pancreatitis
Preventing pancreatitis involves making healthy lifestyle choices:
1. Limit Alcohol Consumption: For people who are at risk, cutting back on or giving up alcohol is essential.
2. Healthy Diet: You can lower the risk by eating a diet high in fruits, vegetables, and whole grains.
3. Control Weight: It is critical to maintain a healthy weight through diet and exercise.
4. Control Blood Sugar: Blood sugar control is crucial for those with diabetes.
Homeopathy as a Complementary Approach
Although traditional medical care is essential in the management of pancreatitis, some people look into alternative therapies like homeopathy. A holistic medical approach, homoeopathy seeks to promote the body’s own healing processes.
Homeopathic Medicines for Pancreatitis
Phosphorus, commonly given as 3-5 pills three times a day, is appropriate for pancreatitis accompanied with greasy, oily feces, vomiting, and a weak, empty feeling in the abdominal cavity.
Arsenicum album is typically taken as three to five pills three times a day to treat pancreatitis that is accompanied with blood, bile, or mucus vomiting.
Colocynth is often taken as three to five pills three times a day and is advised for pancreatitis characterized by excruciating, cutting pain in the belly and jelly-like feces.
Belladonna, given as 3-5 pills three times a day, is effective for pancreatitis, which is characterized by abdominal pain.
It is crucial to remember that homeopathy is an adjunctive therapy and should not be used in place of traditional medical care. In addition to seeing their regular healthcare physician, patients should also speak with a trained homeopathic practitioner.
Foods to Avoid and Improve for Pancreatitis
Foods to Avoid-
1. Alcohol: Get rid of or drastically cut back on alcohol intake.
2. Fried and Fatty Food: Fried and fatty foods should be avoided since they can exacerbate symptoms.
3. Spicy Foods: Spices have the potential to aggravate inflammation and agitate the pancreas.
4. High-Sugar Foods: Too much sugar can interfere with blood sugar regulation.
Foods to Improve-
1. Fruits and Veggies: Consuming a diet high in fruits and vegetables gives you important antioxidants and nutrients.
2. Lean Protein: Choose fish or poultry as lean protein sources.
3. Whole Grains: Rich in fibre, whole grains can help maintain digestive health.
4. Low-Fat Dairy: Opt for dairy products that are low in fat or fat free.
Conclusion: Perfect Pancreas!
In summary, pancreatitis is a difficult ailment that necessitates cautious treatment and alterations to lifestyle. Even while homeopathy can support traditional medical treatments, it is crucial to speak with medical specialists to receive the best possible care.
Notwithstanding the difficulties posed by pancreatitis, people can take charge of their health and strive toward a higher quality of life by being aware of the causes, symptoms, and preventive techniques.
Keep in mind that every patient has a different experience, and that their well being depends on a customised course of therapy and lifestyle.
Reach out to us for a Consultation.
This blog is for information purposes. It’s crucial to note that while homeopathy is a centuries-old practice with many adherents worldwide, always consult a qualified homeopath or medical professional before initiating any treatment.
For any queries, reach out to us at contact@homeopathic.ai